
By Lindsay Mykes
In that same way that a character home gets snapped up the instant it hits the real-estate market because it has “good bones”, good bone health as we age can be a solid indicator of our overall health, quality of life and longevity.
“But bones do not exist in a stable state,” says Deer Lodge Centre physiotherapist Cara Windle. Depending on the choices we make, it’s normal for a healthy older adult to be build up or lose bone mass over time.
The physiotherapists at Deer Lodge Centre are experts in the consequences of poor bone health, including diseases such as osteoporosis and osteoarthritis, largely because the population they serve—adults over the age of 65—commonly have one or both of these two conditions.
In this article, we’ll take a closer look at osteoporosis and osteoarthritis, and show you ways to prevent or manage them.

Bone spongy structure close-ups, normal and with osteoporosis
Osteoporosis: The silent thief
Osteoporosis is a bone disease often referred to as the “silent thief” because it has no symptoms and can be rather advanced by the time it’s detected. The disease causes the bones to become porous, lowering their quality and mass.
“People don’t know that they have osteoporosis until they fracture a bone, or have something called a bone density test,” says Windle.
According to Osteoporosis Canada, ten per cent of Canadians over the age of 45 report having the disease. The numbers may be higher, though, because osteoporosis often goes undetected until secondary issues, such as fractures, present themselves. It’s more prevalent among women than men, especially women over 50, due to differences in hormones and bone frame size.
There’s good news, though, says Windle. “Most of us can prevent osteoporosis by exercising regularly and eating a healthy diet.”
That would mean getting enough calcium and vitamin D. While it’s possible to get your vitamin D from the sun in the summer months, and from dietary sources such as fortified dairy products and orange juice, fatty fish, and egg yolks, Health Canada recommends that all adults over 50 years old take a daily vitamin D supplement of 400 IU. They also recommend 1,000 mg of calcium for adults under 50, or about two servings of milk or alternatives. If you’re over 50, increase your calcium to 1,200 mg, or about three servings of milk or alternatives.
Not everyone will be able to avoid the condition, cautions Windle. “Certain medications lead to osteoporosis, as do certain conditions that don’t allow a person’s muscles to pull or bear weight. If you can’t bear weight, then you don’t tend to build bone.”
If you’re living with osteoporosis, Windle recommends working with a physiotherapist and following a treatment plan to reduce the loss of muscle and bone mass over time.
“People with osteoporosis should talk to their doctor about connecting with an appropriate education program to understand how they can best manage their condition. And they should consult with a physiotherapist to understand safe ways to exercise. Ensure that you’re getting daily weight-bearing activity, with guidance. Start a resistance exercise program in the home or at the gym.”
Windle also advises people living with osteoporosis to learn how to reduce their risk of fractures. She recommends wearing proper footwear, especially in winter, and avoiding leaning forward because flexing the spine can result in fractures of the vertebrae. Medication and diet can also be used to manage the disease.

Pain management is a large component of treating osteoarthritis.
Osteoarthritis: A real pain in the joints
Osteoarthritis is the most common form of arthritis, and it affects a person’s joints. Osteoporosis Canada defines it as “a degenerative joint disease that involves thinning or destruction of the smooth cartilage that covers the ends of bones as well as changes to bone underlying the joint cartilage.” Unlike osteoporosis, which can go undetected, osteoarthritis often announces itself in symptoms such as pain, stiffness and decreased movement of the affected joint.
“This leads to decreased ability to do the activities that you normally enjoy because they become painful,” says Windle.
Forty-five per cent of Canadians over 65 have osteoarthritis, according to Osteoporosis Canada. Women are also more likely to develop osteoarthritis, although researchers don’t know why. A history of joint injuries, family history of osteoarthritis, and performing repetitive tasks can increase your risk of developing osteoarthritis.
Pain management is a large component of treating osteoarthritis. Hot and cold therapy, where heat is used to reduce pain and cold is used to reduce swelling, can be an effective and accessible form of treatment. So, too, can using a gentle range of motion. Windle suggests walking with proper shoes, swimming, or aqua exercise. City of Winnipeg pools have classes specially designed for people with osteoarthritis. Check out the Manitoba section of the Arthritis Society’s website—arthritis.ca—for great exercise options and classes on land and water throughout the city.
When all else fails, joint replacement surgery is another treatment option.

Begin gradually, and, if possible, with some guidance from a therapist.
Best practice for prevention and management
Whether you’re hoping to prevent osteoporosis and osteoarthritis, or looking for ways to live with one or both of these diseases, a good place to start is regular physical activity. We’ve included exercise guidelines from Osteoporosis Canada to help you get started. If you have any concerns about your health, or your ability to perform physical activity, talk to your doctor or a physiotherapist before you begin.
And, please, don’t do too much too soon, Windle cautions.
“Begin gradually, and, if possible, with some guidance from a therapist. If you overdo it, you’ll end up with even more pain, which will only set you back, instead of move you forward.”
Exercising for Healthy Bones
| TYPE | FREQUENCY | BENEFITS |
Strength training
| At least twice a week |
|
Balance training
| Daily |
|
Weight-bearing aerobic physical activity
| Most days of the week |
|
Posture training
| Always! |
|
Source: www.osteoporosis.ca/osteoporosis-and-you/exercise-for-healthy-bones/
Recent News
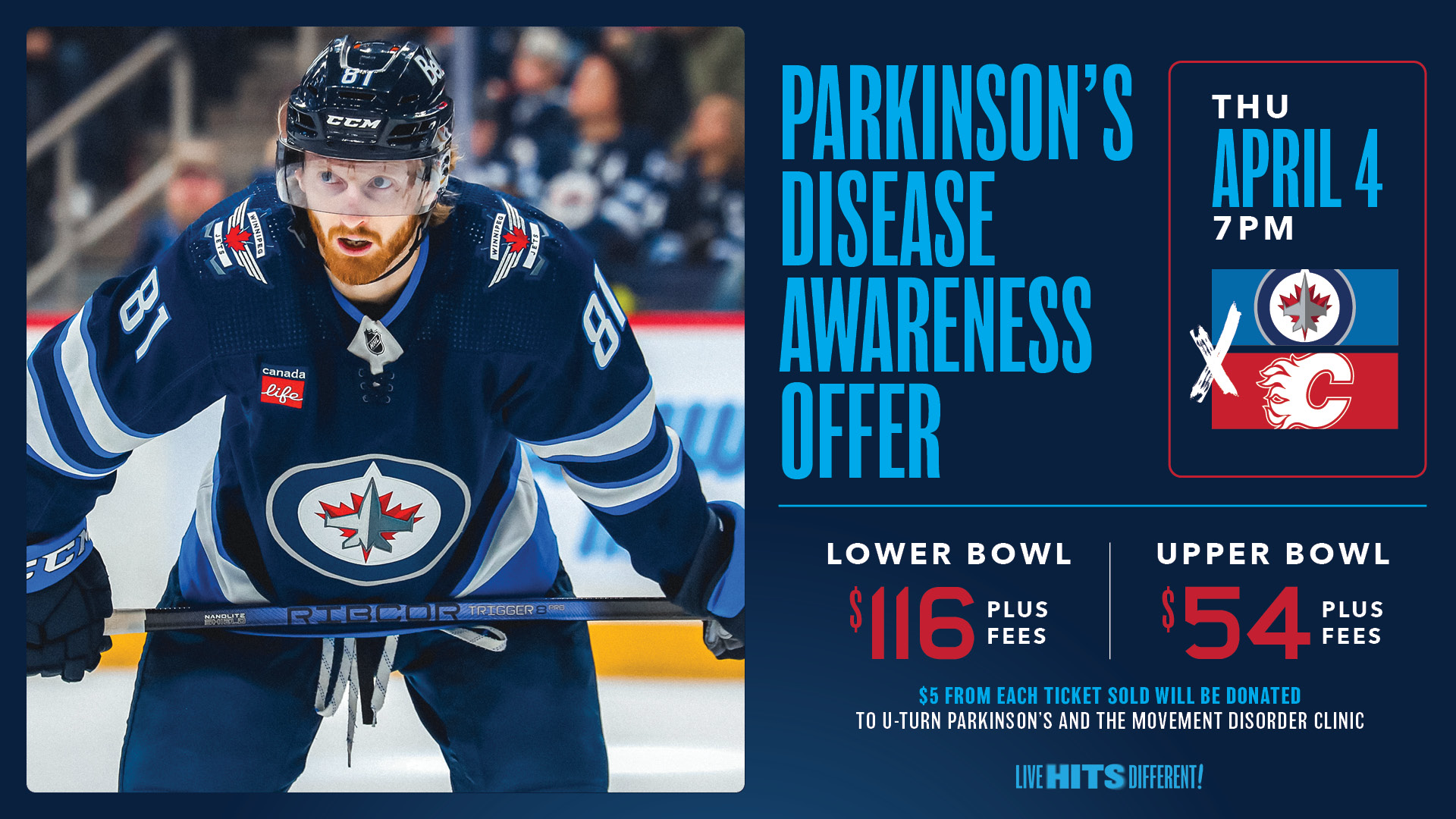
Winnipeg Jets Parkinson’s Disease Awareness Game!

Volunteer Profile: Carole Grier

